Operating Room Temperature & Humidity Monitoring System
How E-Control Systems Works for Operating Room Environmental Monitoring
E-Control Systems offers effective solutions for monitoring and controlling operating rooms in hospitals to ensure optimal conditions for surgeries. Our system utilizes wireless sensors placed strategically within the operating room to monitor crucial parameters such as temperature, humidity, air quality, and differential pressure in real-time.
The collected data is transmitted to a centralized system for analysis and action. In the event of any deviations from the desired conditions, E-Control Systems triggers instant alerts through email, SMS, or mobile app notifications, notifying relevant personnel. This enables prompt intervention to address any issues that may impact the safety and success of surgical procedures.
Our systems provide comprehensive data logging and reporting features, creating a historical record of the operating room’s environmental conditions. This data can be accessed and analyzed for compliance purposes, quality control, and process improvement. By offering real-time monitoring, instant alerts, and data-driven insights, E-Control Systems ensures that operating rooms maintain optimal conditions for surgeries, contributing to the safety and well-being of patients.
E-Control Systems Features for Hopsital Operating Room Monitoring
What makes E-Control Systems stand out? Our sensors and intelligates can monitor any aspect of your Operating Room business 24/7.
What Sets Our Operating Room Monitoring Apart from Other Options in the Market?
Our operating room monitoring solution stands out in the market due to its reliability and advanced features. Using wireless sensors strategically placed within the operating room, our system provides real-time monitoring of crucial parameters such as temperature, humidity, air quality, and differential pressure. This ensures that the operating room maintains optimal conditions for successful surgeries.
What sets our solution apart is the comprehensive data logging and reporting features it offers. This allows for the creation of a historical record of environmental conditions within the operating room, enabling analysis for compliance, quality control, and process improvement purposes. Furthermore, our system’s ability to trigger instant alerts via email, SMS, or mobile app notifications in case of deviations ensures prompt intervention to address any issues and maintain the safety of patients. With its reliability, advanced features, and focus on data-driven insights, our operating room monitoring solution provides a superior option for ensuring optimal conditions during surgical procedures.
Our Operating Room Customers Include:
Operating Room Environmental Monitoring Equipment
Operating Room Temperature Monitoring FAQ's
What is the standard temp for an operating room?
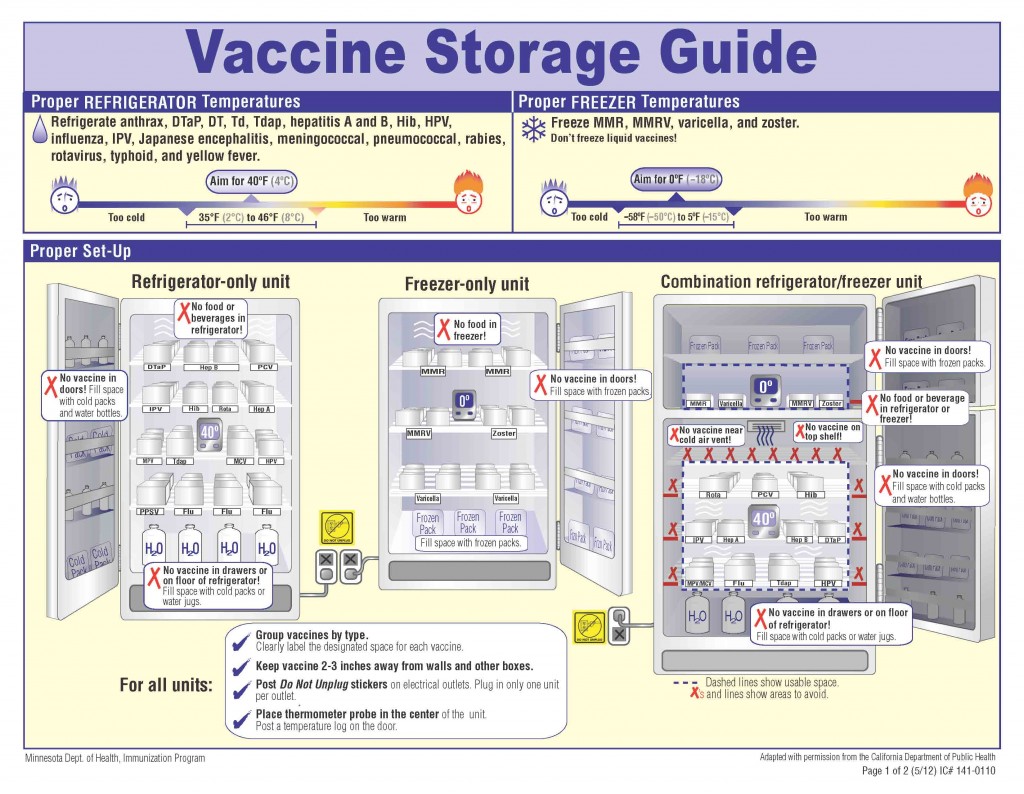
The standard operating room temperature should be maintained between 68°F and 73°F. This range helps ensure a comfortable environment for both the surgical team and the patient while helping to control the spread of infections. It's important to maintain this temperature range to support the sterility of the environment and the functionality of medical devices and supplies that may be sensitive to temperature fluctuations.
What are the AORN guidelines for operating room temperature?
The Association of periOperative Registered Nurses (AORN) provides operating room temperature guidelines to ensure patient safety and comfort while maintaining optimal conditions for staff and surgical equipment. According to AORN guidelines, the recommended temperature in an operating room should be maintained between 68°F and 75°F. This range controls microbial growth, provides comfort for the patient (who may be more susceptible to hypothermia during surgery), and ensures a comfortable working environment for the surgical team members.
Humidity levels are also an important factor. Aorn standards for operating room temperature and humidity recommend relative humidity in operating rooms be maintained between 20% and 60%. An operating room temperature and humidity policy balances the need to minimize infection risks, managing patient and staff comfort, and protecting medical equipment.
What happens if the humidity is too high in an operating room?
If the humidity in an operating room is too high, issues can arise that may compromise the safety and effectiveness of surgical procedures:
- Increased Risk of Infection: High humidity can promote microbial growth, including bacteria and fungi. This increases the risk of infections, particularly surgical site infections, which are critical to avoid in a sterile environment like an operating room.
- Compromised Sterility: Excessive moisture can affect the sterility of surgical instruments and other supplies. For example, high humidity can cause condensation on sterile packages, potentially compromising their integrity and leading to contamination.
- Equipment Malfunction: Many medical devices used in surgeries are sensitive to environmental conditions. High humidity can lead to malfunctioning of these devices by causing condensation or corrosion on electronic components, which can disrupt surgeries and pose safety risks.
- Comfort and Visibility Issues: High humidity levels can make the environment uncomfortable for the surgical team, potentially impairing their ability to perform tasks efficiently. It can lead to fogging of surgical glasses and scopes, reducing visibility during procedures.
What are WHO guidelines for room temperature?
The World Health Organization (WHO) provides general guidelines for room temperatures in healthcare settings, emphasizing the prevention of patient hypothermia during surgery. While specific temperatures are not detailed, the WHO supports maintaining operating room temperatures between 68°F and 75°F, aligning with practices to reduce infection risks, ensuring equipment functionality, and providing comfort for both patients and healthcare staff. Temperature settings should meet local regulations and support overall healthcare objectives.
Do operating rooms have to be cold?
Operating rooms are kept cooler than normal room temperature, but they don't necessarily have to be "cold." It's important to balance these needs with the comfort of the patient, who may be more susceptible to hypothermia, especially during lengthy operations. This is why ideal operating room temperature is carefully regulated based on the type of surgery, the condition of the patient, and the preferences of the surgical team.
What temperature is hypothermia in the operating room?
Hypothermia in the operating room is generally defined as a body temperature lower than 36°C (96.8°F). During surgery, it's important to monitor and maintain the patient's body temperature to prevent hypothermia, which can lead to various complications like increased risk of infection, prolonged hospital stays, and adverse cardiac events.
To avoid hypothermia, operating rooms are equipped with various warming devices and techniques, like warmed intravenous fluids, warming blankets, and forced-air warming systems, to help maintain the patient's body temperature within a safe range. These ensure the patient's temperature does not fall below 36°C, especially during lengthy surgeries or procedures involving significant exposure of body cavities, which increase the risk of heat loss.
Why is operating room temperature important?
Temperature in the operating room is important because it controls infection by reducing bacteria, and maintains a sterile environment. Proper temperature management is vital for preventing hypothermia in patients, which can lead to increased blood loss, higher infection rates, and prolonged recovery periods. A cooler temperature ensures the comfort and optimal performance of the surgical team, who often wear protective clothing that can become uncomfortably warm during lengthy procedures. Many medical devices used in surgeries perform best in cooler conditions, making temperature control essential for equipment reliability and effectiveness. Operating room temperature is meticulously regulated to ensure safety and efficiency during surgeries.
What is the best way to measure operating room temperature?
The best way to measure temperature of an operating room is by using accurate and reliable temperature monitoring systems that ensure consistent readings and maintain the required standards for a sterile surgical environment. Here’s how operating room temperatures are typically measured and maintained:
Remote Monitoring Systems: Implementing remote monitoring solutions allows for real-time temperature tracking and alerts if temperatures deviate from set parameters. This technology helps quickly address any issues that might compromise the sterile environment.
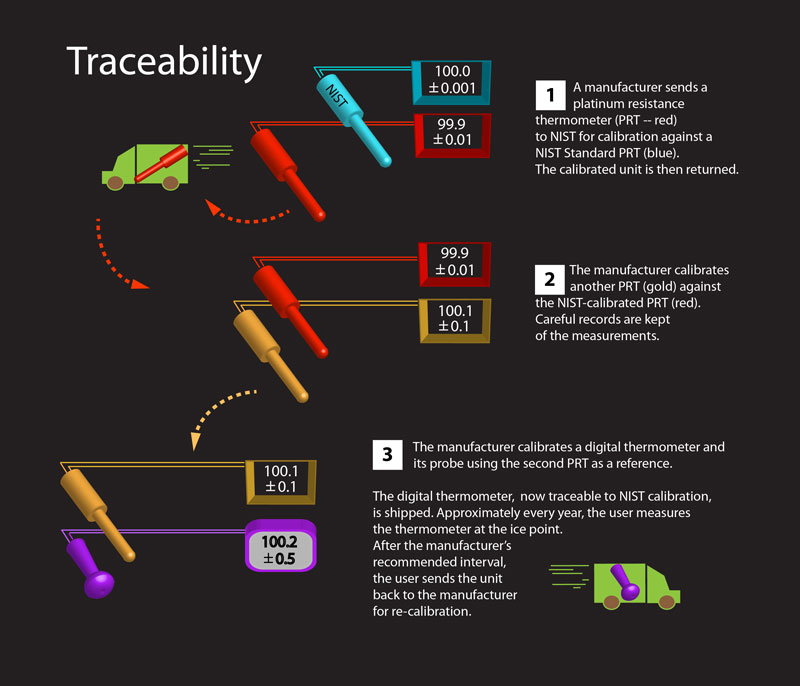
What instrument measures operating room temperature?
The instrument used to measure operating room temperature is a digital thermometer. Digital thermometers are preferred because they can provide precise and quick temperature readings. Digital thermometers can be placed at multiple locations within the operating room to ensure consistent temperature throughout the space. They can be integrated into the room’s HVAC system to continuously monitor and adjust the temperature as needed, ensuring it remains within the recommended range for a sterile and safe surgical environment. Thermometers can be part of a broader environmental monitoring system that also tracks humidity and other critical parameters.
What types of hospital operating room monitoring equipment are used to maintain compliance?
Advanced hospital operating room monitoring equipment helps hospitals comply with regulatory standards when managing air quality, temperature, and humidity levels. Sensors are installed in surgical settings to ensure sterile conditions in operating rooms. Airflow monitors are used to prevent the risk of infections from spreading. When they use a monitoring system with automated logging capability, it allows them to capture and store valuable information that can prove they’re using safe practices when an official audit or inspection occurs. Hospitals need advanced monitoring systems to ensure safe surgical practices and compliance in their operating rooms.
How do hospitals maintain and manage an operating room temperature and humidity log?
Hospitals maintain an operating room temperature and humidity log 24/7 with the help of automated sensors that connect to central monitoring systems. The sensors record data and store it electronically so staff can ensure operating room conditions are safe. Immediate corrective action can be taken when a deviation triggers an alert. This ensures the operating room is a safe place to perform surgery as needed, while supporting compliance.
What are the standard operating room temperature and humidity requirements?
To keep patients safe and ensure equipment that’s sensitive to changing temperatures in the surgical setting functions properly, operating room temperatures should be kept between 68°F and 73°F. Humidity levels should fall between 20% and 60% to prevent infections from spreading and protect surgical tools. These temperatures also keep the surgical team comfortable while they’re operating. When hospitals monitor temperatures with a temperature monitoring system, they ensure the operating room has the safest possible surgical environment for patients.
How can automated procedure room monitoring systems improve hospital efficiency and safety?
Automated procedure room monitoring systems provide more reliable documentation than handwritten logs, especially for audits and inspections. Sensors monitor air quality and the temperature of each room, and provide alerts when changes occur. Because data is recorded and stored, these efficient systems eliminate human error, plus staff can now concentrate on ensuring patients are safe and cared for, instead of completing paperwork. Due to fewer interruptions, surgeries can be completed efficiently and on time in a sterile space, avoiding delays.
What should an operating room temperature and humidity policy include?
A hospital operating room temperature and humidity policy should emphasize patient safety and maintain regulatory rules to create a sterile surgical environment. It should require the use of automated sensors and data logging systems, and assign staff to perform daily checks to ensure consistent compliance and accountability, so surgeries are safely completed. The hospital policy should also list corrective actions that should be taken when temperature and humidity deviations occur. When the hospital defines roles and workflows, it will ensure consistent environmental control in every surgery for better patient outcomes.
How long should hospitals retain operating room environmental monitoring records?
When a hospital keeps environmental records, it provides them with a record of operating room conditions if questions arise about surgeries or equipment performance. Keeping these records for several years can help identify recurring temperature and humidity issues and patterns to strengthen infection control. E-Control Systems archives valuable data automatically and keeps it in an organized archive that’s easy to retrieve. This approach ensures the hospital has documentation for regulatory audits available that proves it always uses safe practices in operating rooms.